I learned about U=U in 2019.
Not in 2016 when the message officially launched. Not at the beginning. I learned about it three years later, when the science was already clear and the evidence overwhelming. And what struck me immediately wasn’t the data. It was the disconnect.
Doctors had the science.
The world hadn’t caught up.
People living with HIV are still being treated as dangerous. Still criminalized. Still framed as a problem to manage rather than people to respect. The science says something radical and simple. Undetectable equals untransmittable. Zero risk. Full stop. But culture, law, and everyday beliefs are still operating on fear.
That gap changed me.
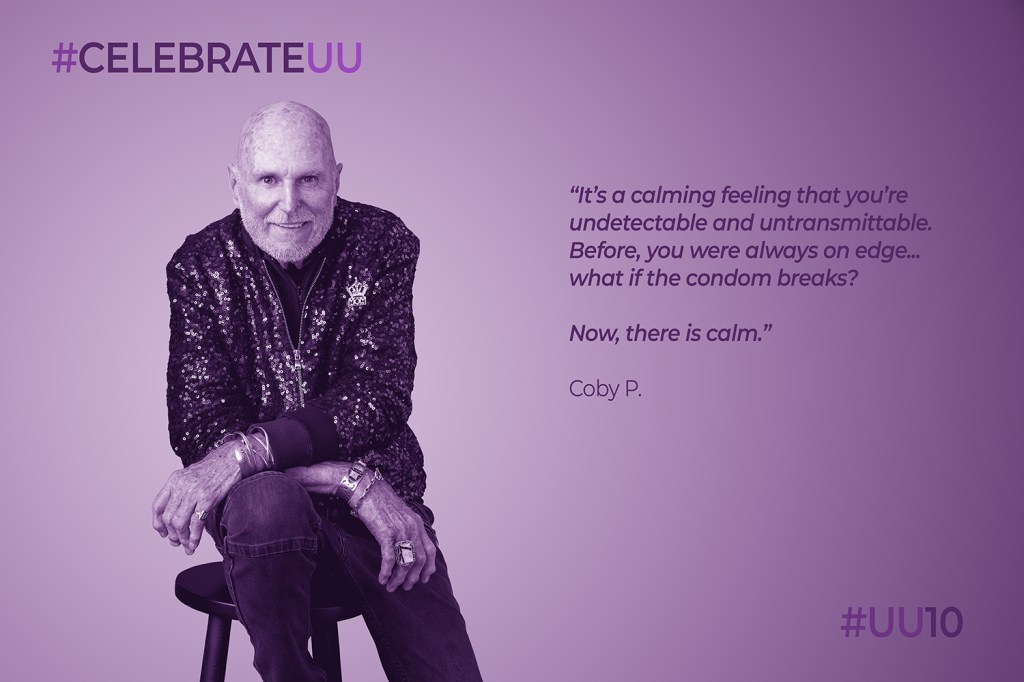
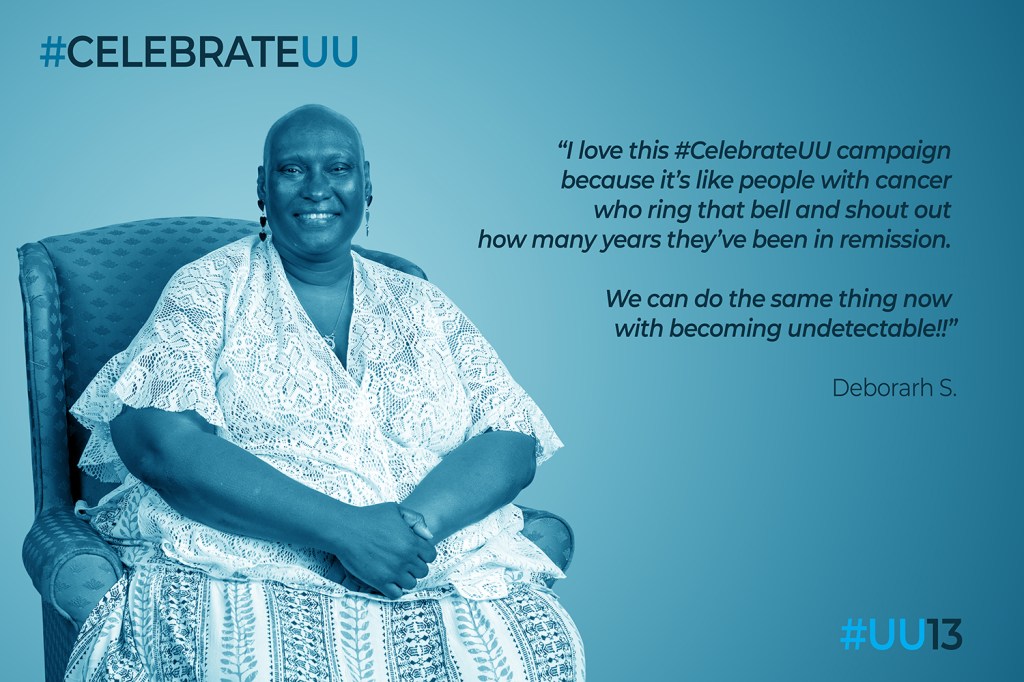
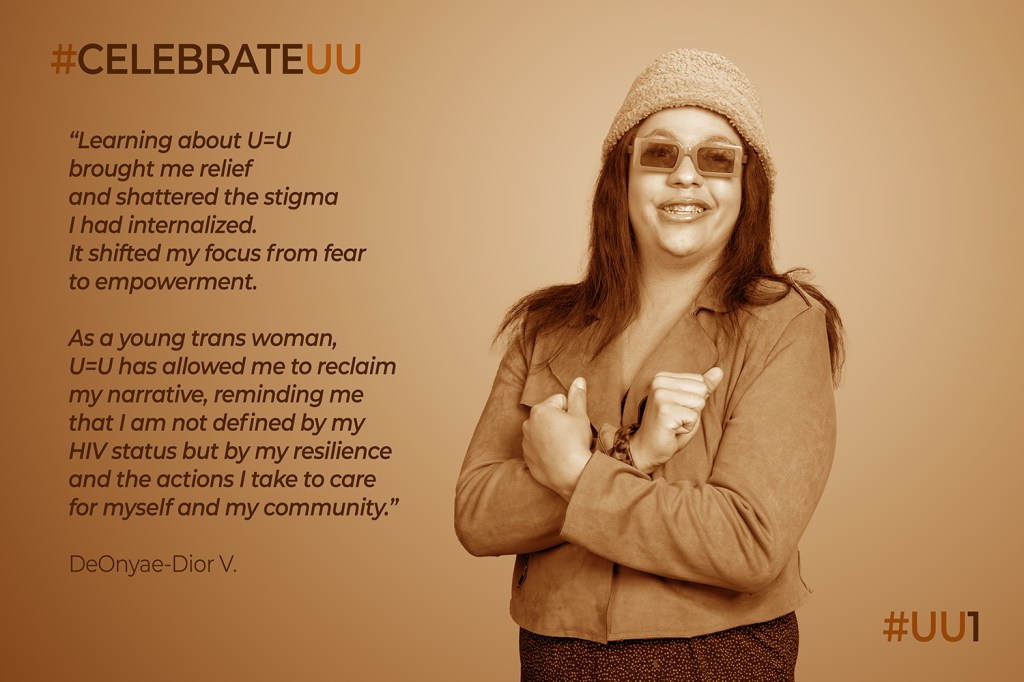
Later that year, I launched #CelebrateUU, not as an education campaign, but as a visibility project. I didn’t want to explain U=U. I wanted people to see it. Real people. Real faces. Real intimacy. Because stigma doesn’t dissolve through statistics alone. It dissolves when humanity becomes undeniable.
Over the years, I’ve watched U=U do incredible things.
When people receive clear, confident U=U information, it changes how they see themselves. It restores sexual confidence. It reframes treatment from obligation to empowerment. It opens the door to honesty, joy, and possibility. In clinical settings where providers speak clearly and without hedging, trust grows. Fear recedes. People breathe again.
But ten years in, it’s also clear where U=U hasn’t gone far enough.
U=U didn’t fail. But its impact has been uneven because belief spread slower than evidence.
Too many providers still hedge.
Too many public messages flatten U=U into a slogan.
Too many rural and marginalized communities are left behind.
Too many laws still treat people with HIV as a risk, not as people living with a managed condition.
And in the middle of this, a real and complicated concern has emerged. The fear that U=U creates a viral divide.
That concern deserves honesty, not avoidance.
A person’s value is not determined by viral load. Full stop. When someone can’t reach viral suppression, that is very often a failure of systems, not individuals. Housing instability. Mental health. Poverty. Trauma. Access gaps. Stigma itself. These are not personal shortcomings. They are structural barriers.
And the vast majority of people who are not virally suppressed still care deeply about preventing transmission. They take precautions. They disclose. They navigate risk thoughtfully and responsibly, often with far less support than they deserve.
But here’s the hard truth we can’t avoid.
Fear of creating a viral divide cannot be used to weaken or hide settled science.
The answer to inequity is not diluting the truth. It’s fixing the systems that keep people from benefiting from it. When we hedge U=U out of discomfort, we don’t protect people. We reinforce stigma. Worse, we create space for bad policy.
This matters because stigma doesn’t just live in attitudes. It lives in law.
U=U exposes how outdated HIV criminalization laws are, but science alone doesn’t repeal bad laws. When institutions hedge on U=U, they reinforce the idea that people with HIV are inherently dangerous, and that shows up in courtrooms, sentencing, and statutes.
In recent years, my work has shifted toward implementation. Grounded in U=U University, which clearly defines the science, I’ve focused on the question that ten years of U=U now demands: What happens after awareness?
Knowing the science is not the same as practicing it. When providers hesitate, when systems stay silent, stigma survives. And patients pay the price.
If a provider can’t explain U=U clearly, confidently, and consistently, then the promise of U=U remains theoretical for the people who need it most.
Ten years later, U=U has proven what’s medically possible. The virus can be rendered untransmittable. Fear no longer belongs in the science.
The work now is alignment.
Aligning healthcare with evidence.
Aligning law with reality.
Aligning public messaging with dignity.
Until our systems behave as if they believe what the science already tells us, U=U remains true, but its promise isn’t fully realized.
And that’s where the next decade begins.